Colorectal cancer has become the leading cause of cancer death in Americans under 50, even as under-50 cancer mortality overall has declined. The American Cancer Society’s new analysis (published January 22, 2026) reports colorectal cancer mortality in younger adults rising about 1.1% per year since 2005, advancing it to the top cancer killer in 2023 for this age group.
In parallel, the federal posture on wireless “certainty” is shifting. HHS has announced a new study on cellphone radiation, and multiple reports note the FDA removed webpages containing older categorical safety language while HHS undertakes this research.
This is not an official declaration that phones are proven dangerous; it is a public acknowledgement that messaging should not outpace evidence, and that gaps remain worth examining with modern technologies and modern exposure patterns.
At the same time, major institutions still state that evidence to date has not established a causal link between cellphone use and cancer in humans, underscoring that the debate is about uncertainty and study quality, not settled proof.
RF Safe’s position is straightforward: when a cancer trend is worsening in the young, and a ubiquitous exposure plausibly targets the relevant anatomy, the correct scientific response is not dismissal—it is well-powered replication.
2) The epidemiologic “signal” that warrants replication (not overinterpretation)
A key reason the “below-the-waist” hypothesis is scientifically interesting is that it makes a specific prediction, not a vague one.
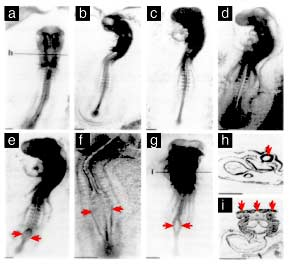
Dr. De-Kun Li (Kaiser Permanente) proposed that carrying an actively transmitting smartphone below the waist could contribute to early-onset colorectal cancer (EOCRC). In a small pilot case-control study (reported in conference context and science reporting), phone-carrying below the waist was associated with higher EOCRC odds; the association was reported as stronger when the phone was carried on the same side as the tumor (“ipsilateral” carrying), and weaker when carried on the opposite side (“contralateral” carrying).
That laterality detail matters because it is testable and, if reproduced, would be harder to explain by broad lifestyle confounding alone. But the pilot’s limitations (small sample, recall bias risk, and the need for preregistered replication) are exactly why it must be treated as a hypothesis generator, not a public verdict.
RF Safe’s claim is not “this proves causation.” RF Safe’s claim is: “This is specific enough—and the stakes are high enough—to justify serious replication with objective exposure measurement.”
3) The exposure geometry: why pocket carry is a different biological question than “cell phones and brain tumors”
Most public debate about phones and cancer has focused on brain tumors because calls place the antenna near the head. That is not the dominant use pattern anymore.
Modern smartphones spend thousands of hours:
-
pressed against the abdomen/pelvis in front pockets,
-
against the lower back in back pockets,
-
directly against skin via leggings, belts, and waistbands,
-
intermittently transmitting for network registration, data sync, messaging, background apps, Wi-Fi, Bluetooth, and location services.
This matters because RF exposure is highly distance-dependent in the near field. The highest energy deposition is closest to the device—precisely the circumstance created by pocket carry.
Even if the average power is low, the cumulative hours can be enormous over a decade. The “dose” question cannot be dismissed simply because the signal is non-ionizing. It is a question of proximity, repetition, and biological response over time—especially when the exposure is directed into the abdomen/pelvis where portions of the colon and rectum are anatomically relevant to EOCRC.
4) A mechanistic bridge: how RF could plausibly act as a contributing factor without being the sole cause
RF Safe argues that the most credible framing is not “RF causes EOCRC by itself,” but “RF may be a co-factor that shifts tissue biology toward higher risk in susceptible conditions.”
Here are the most defensible mechanistic avenues—each presented as testable hypotheses, not settled conclusions:
A) Chronic micro-stress signaling and loss of cellular “fidelity”
EOCRC is increasingly described as a disease where the normal controls on proliferation, repair, and immune surveillance fail earlier than expected.
RF Safe’s S4–MITO–spin framing is an attempt to describe how low-level electromagnetic exposures could add “noise” to biological control networks—particularly through pathways involving membrane voltage sensing (ion-channel gating), downstream mitochondrial stress/ROS signaling, and redox chemistry. This is not yet a clinically validated framework; it is a research hypothesis about how “upstream” signaling disruption could have “downstream” consequences over years.
What gives this category of mechanism legitimacy is not that it is proven end-to-end, but that biology does respond to chronic stressors via inflammation, oxidative signaling, and altered gene expression—pathways commonly implicated in cancer biology.
A concrete example that RF exposure can correspond with epigenetic changes in colon-related contexts exists in experimental literature (not definitive for real-world causation, but supportive of biological plausibility).
Testable prediction: pocket-carry heavy users will show measurable differences in validated biomarkers (oxidative stress, inflammatory cytokines, DNA damage response signaling, methylation patterns) in tissue-adjacent or systemic assays, after controlling for confounders.
B) The microbiome as a missing link (and why RF is a plausible modifier)
A major scientific development in EOCRC research is the strengthening evidence that early-life exposures to microbiome-derived mutagens may contribute to risk.
A 2025 Nature study analyzing 981 colorectal cancer genomes across 11 countries reported that mutational signatures consistent with exposure to colibactin-producing bacteria were substantially more common in early-onset cases, suggesting early-life microbial mutagen exposure may contribute to EOCRC trends.
RF Safe’s hypothesis does not need to compete with this; it can integrate with it:
-
If EOCRC risk is partially driven by microbiome mutagens, then anything that plausibly affects gut barrier integrity, immune tone, autonomic signaling, or inflammatory state could act as a modifier—altering susceptibility to microbial toxins or the body’s ability to constrain them.
Testable prediction: higher below-the-waist RF proximity exposure correlates with reproducible differences in microbiome composition/function and gut permeability markers, and these differences predict EOCRC-relevant mutational signatures or precancerous lesion prevalence.
C) Why animal data keeps the door open—even if it does not answer EOCRC directly
The U.S. National Toxicology Program (NTP) performed large animal studies and reported tumor findings associated with high RF exposure (e.g., clear evidence of malignant schwannomas in the hearts of male rats).
Those studies used exposure conditions that do not map neatly onto everyday smartphone pocket carry, and they do not “prove” EOCRC risk. But they do defeat the overly simplistic claim that “non-ionizing RF has no carcinogenic relevance under any circumstances.” They justify continued mechanistic work—especially as consumer technologies and modulation patterns evolve.
D) Classification and uncertainty: why “possible carcinogen” does not equal “proven safe”
IARC has classified radiofrequency electromagnetic fields as “possibly carcinogenic to humans” (Group 2B), reflecting credible signals but unresolved confounding/causality.
That classification, combined with (1) a worsening EOCRC trend and (2) a plausible exposure geometry that targets the abdomen/pelvis, is sufficient to justify large, modern, preregistered studies focused on below-the-waist carry patterns.
5) The most important scientific caveat: confounding is real, so the next studies must be better
The strongest critique of the pocket-carry hypothesis is that it may be a proxy for other modern risk factors:
-
sedentary time and screen time,
-
diet patterns,
-
obesity and metabolic syndrome,
-
alcohol consumption,
-
sleep disruption,
-
socioeconomic and healthcare access factors.
This is exactly why RF Safe’s advocacy should be pointed at study design, not rhetoric.
If we want an answer that clinicians and regulators can trust, the next wave of studies must include:
-
Objective exposure data (phone telemetry, carry-position tracking, app/network activity logs), not just recall surveys.
-
Laterality pre-specification (tumor location and side-of-carry hypotheses preregistered).
-
Dose modeling that reflects real-world behavior (signal conditions, duty cycle, proximity, clothing/body contact).
-
Robust confounder control (BMI, diet, activity, alcohol, smoking, sleep, SES, screening history).
-
Mechanistic substudies (microbiome, inflammation, oxidative stress, epigenetics).
-
Replication across populations and independent analytic teams.
That is how the field separates “interesting signal” from “false correlation.”
6) What RF Safe can responsibly recommend now (precaution without panic)
While science catches up, the public can reduce an uncertain exposure at low cost—without claiming it prevents cancer:
-
Avoid storing an actively connected phone pressed against the abdomen/pelvis for long durations.
-
Carry in a bag when practical; if pocket carry is unavoidable, increase distance (even small distance changes matter).
-
Use speakerphone or a wired option for longer calls.
-
Recognize phones may transmit more aggressively in poor reception.
And separately—because it is proven lifesaving—RF Safe should continue to amplify screening and symptom urgency consistent with clinical guidelines (e.g., screening beginning at 45 for average risk per USPSTF, earlier for higher-risk histories).
The advocacy conclusion
EOCRC is now killing more younger Americans than any other cancer.
HHS is reopening the question of wireless health impacts and has initiated a new study while prior categorical FDA language has been removed from some webpages.
That combination demands a serious, funded scientific response. A small, laterality-specific pilot signal—like below-the-waist, ipsilateral carry—should not be mocked or ignored. It should be replicated at scale with modern exposure measurement, modern biology, and transparent preregistration.
If the hypothesis is wrong, society deserves to know decisively. If it is partially right, society cannot afford to learn that a decade late.