—and “we don’t know why” is no longer acceptable
For three decades, the U.S. has watched a hopeful trend take hold: cancer deaths in people under 50 have fallen dramatically. And yet, one disease has moved in the opposite direction—quietly at first, then unmistakably.
Colorectal cancer is now the leading cause of cancer death in Americans under 50.
That single fact should stop policymakers, clinicians, and researchers in their tracks—not only because it is tragic, but because it is diagnostically and scientifically indicting. It signals that a growing number of younger adults are still being missed until the disease is advanced, and that the forces driving this rise remain inadequately understood.
Public health does not get to accept “mystery” as an endpoint.
A paradox that demands a wider lens
In people under 50, overall cancer mortality has declined substantially since 1990. Lung cancer deaths have fallen. Breast cancer deaths have fallen. Leukemia deaths have fallen. Brain cancer deaths have fallen. But colorectal cancer mortality has increased year after year since the mid-2000s—lifting it from a lower-ranked cause of cancer death in younger adults to the number one position by 2023.
A society can celebrate progress against cancer broadly and still be failing a generation in one very specific, very preventable way.
The immediate priorities are clear and non-negotiable:
-
Earlier detection (including acting promptly on symptoms and removing barriers to screening).
-
Faster diagnosis in primary care and urgent care settings.
-
Better clinician awareness that colorectal cancer is no longer “rare” in younger adults.
But even perfect screening compliance will not answer the most consequential question: Why is this happening?
Traditional risk factors do not fully explain the trend
Researchers have associated early-onset colorectal cancer with multiple well-established risk factors: obesity, physical inactivity, dietary patterns, alcohol use, and other metabolic and inflammatory drivers. Many of these factors have worsened in modern life.
And yet, even when these are accounted for, the pattern has continued to deepen across multiple affluent countries. That has pushed scientists to ask whether additional, under-measured exposures—newer, pervasive, and biologically plausible—are contributing.
The uncomfortable truth is that modern epidemiology often studies what is easy to measure, not what is most ubiquitous.
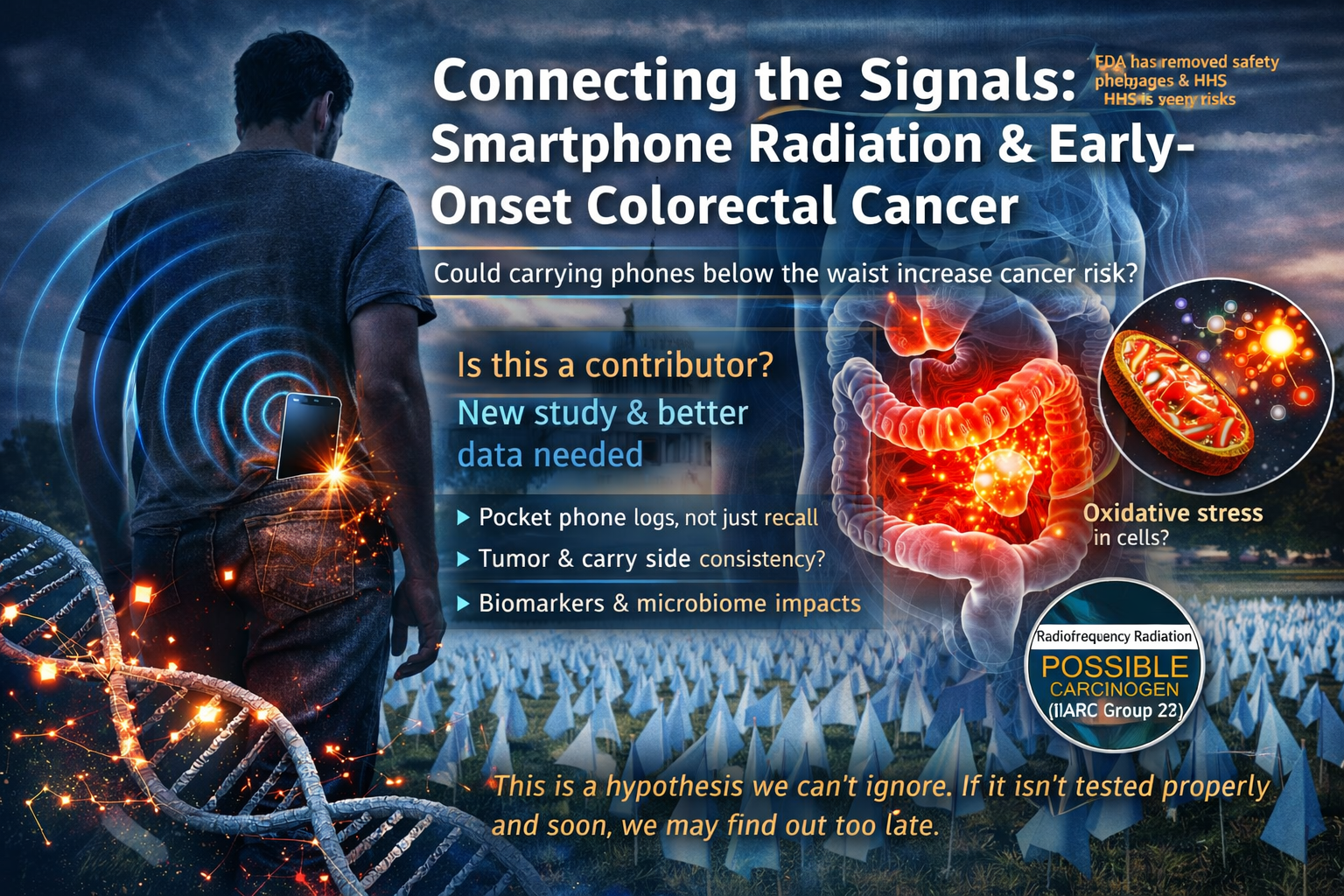
A provocative signal: phones carried below the waist
One emerging hypothesis sits right at the intersection of ubiquity and under-measurement: radiofrequency (RF) exposure from cell phones carried against the body—specifically below the waist.
Epidemiologist Dr. De-Kun Li of Kaiser Permanente has argued that this is a plausible risk factor worth formal investigation because it involves:
-
A near-universal exposure (smartphones),
-
In a specific anatomical context (abdomen/pelvis),
-
With a behavioral pattern that has become routine (hours per day, for years),
-
And a disease site that is rising sharply in younger adults (colon/rectum).
In a small pilot study (50 early-onset colorectal cancer cases and 50 matched controls), Li reported that people who carried a phone below the waist were substantially more likely to have tumors than controls. Even more striking, the association appeared strongest when the phone was carried on the same side as the tumor (an “ipsilateral” pattern). In a subgroup analysis, very high cumulative hours of left-side phone carrying corresponded with a markedly elevated odds estimate for left-sided tumors.
This is exactly the kind of finding that creates controversy for a reason: it is not definitive—but it is specific enough to test.
And that specificity matters.
A hypothesis that predicts laterality (same-side carry vs opposite-side carry) is not just waving at a vague correlation. It is proposing a pattern that, in principle, can be validated or refuted with better exposure measurement, larger samples, and rigorous bias controls.
The scientific posture should be: “replicate, don’t ridicule”
There are obvious reasons for skepticism:
-
The pilot sample is small.
-
Self-reported carrying habits are vulnerable to recall bias.
-
Confounding factors (occupation, lifestyle, sedentary time, obesity, diet) can distort results.
-
Multiple comparisons and subgroup analyses can inflate apparent signals.
Those critiques are real—and they are precisely why the correct response is not dismissal. The correct response is replication.
Because if the signal disappears under stronger study design, the public deserves to know that, too.
Mechanisms: not settled, but no longer dismissible as “only heating”
This is where much of the public debate becomes distorted.
RF from phones is non-ionizing radiation. It does not break DNA bonds the way ionizing radiation (X-rays, gamma rays) can. For years, the dominant regulatory framing has treated tissue heating as the primary established biological interaction.
But the scientific record is more complicated than the simplistic claim that “there is nothing to see here.”
The National Toxicology Program (NTP), headquartered at the National Institute of Environmental Health Sciences (NIEHS), conducted major animal studies and reported tumor findings in rats exposed to high levels of radiofrequency radiation (RFR), including clear evidence of malignant schwannomas in the hearts of male rats and some evidence of malignant gliomas in the brains of male rats. These animal results do not translate cleanly to real-world human use—exposures differed in duration, intensity, and distribution—but they do challenge the idea that biological concern begins and ends with obvious heating.
This is not proof that phones cause colorectal cancer. It is proof that the biology is not trivial enough to justify complacency.
A mechanistic “bridge” being proposed: the S4–MITO–spin framework
RF Safe and other advocates have pushed a mechanistic synthesis they describe as the S4–MITO–spin framework, aiming to connect three proposed interaction pathways:
-
S4: effects on voltage-sensing segments of voltage-gated ion channels,
-
MITO: downstream mitochondrial stress and reactive oxygen species (ROS) signaling,
-
spin: radical-pair / spin-dependent chemistry that could, in theory, modulate redox biology under certain conditions.
This is not mainstream regulatory doctrine, and it should not be presented as a proven causal map. But it is a relevant feature of the current scientific landscape because it highlights a key point: there are testable mechanistic hypotheses on the table that go beyond “does it heat tissue?”
Mechanistic plausibility should not be used as a substitute for epidemiology—but it can be used to design better studies:
-
What biomarkers should be measured?
-
What tissues are plausible targets?
-
What exposure patterns matter (distance, laterality, duration, modulation, duty cycle)?
-
What “downstream” pathways would be expected if the hypothesis were true?
In other words: the mechanistic debate can be reframed as a research agenda rather than a talking-point war.
Federal messaging is shifting—because the question is not closed
The policy environment has also shifted in a way that matters for advocacy: the U.S. Department of Health and Human Services has announced a new study on cellphone radiation, and reporting indicates the FDA removed older webpages that conveyed categorical reassurance, describing them instead as containing “old conclusions,” while the broader review proceeds.
That does not mean the government has declared phones dangerous. It means something more important for scientific integrity: federal agencies are acknowledging that the public-facing certainty level should match the actual certainty of the evidence.
At the same time, the FDA still summarizes its position that the “weight of scientific evidence” has not linked cell phone RF exposure to health problems, reflecting that the official consensus has not simply flipped overnight.
That tension—between past confidence and present re-examination—is exactly why stronger research is needed now, not later.
What “real” research would look like (and why it must be funded)
If early-onset colorectal cancer is now the top cancer killer in younger Americans, then the research response should match that urgency. For the phone-below-the-waist hypothesis (and other under-measured modern exposures), that means studies designed to survive criticism:
-
Large, multi-site replication
Thousands of cases, not dozens—across diverse populations and healthcare systems. -
Objective exposure measurement
Move beyond memory-based surveys where possible: phone logs, usage analytics, wearable proximity data, and validated questionnaires. -
Laterality and anatomy-aware endpoints
Tumor location (left vs right colon, rectum) should be pre-specified—not an afterthought. -
Confounder discipline
Rigorous adjustment for BMI, diet, alcohol, smoking, physical activity, sedentary time, occupation, and screening history. -
Dose modeling that reflects real carry behaviors
Not just “phone ownership,” but pocket carry vs bag carry, duration, signal strength variability, and proximity. -
Mechanistic substudy layers
Microbiome profiling, inflammatory markers, oxidative stress markers, metabolomics—tied to exposure profiles. -
Preclinical models that mirror real-world geometry
Not only whole-body exposure, but localized abdominal/pelvic exposure patterns and contemporary signal characteristics. -
Transparent preregistration and independent analysis
A study that only one “side” trusts is not a public health study. Protocol preregistration and independent replication are essential.
This is not exotic science. It is competent modern epidemiology—properly funded and properly designed.
Precaution without panic: what the public can do while science catches up
Advocacy does not have to choose between complacency and hysteria.
Even if the phone-carry hypothesis ultimately proves false, there are low-cost, low-disruption behaviors that reduce RF exposure for those who want to take reasonable precautions while evidence evolves:
-
Avoid storing an active phone pressed against the abdomen/pelvis for long durations.
-
Prefer bags, backpacks, or off-body carry when feasible.
-
Use speaker mode or wired options for longer calls.
-
Be mindful that a phone working harder in poor reception can alter transmission behavior.
None of this replaces screening, and none of it should be framed as a guarantee of protection. It is simply risk management under uncertainty—common in public health when exposures are widespread and outcomes are serious.
The advocacy point that matters most
Early-onset colorectal cancer is not a niche trend. It is now the leading cancer killer of younger Americans.
When that happens, the default public health posture must be:
-
Measure more.
-
Study harder.
-
Fund replication.
-
Update guidance when evidence changes—without political theater, without industry capture, without activist overreach.
If cell phone carrying habits turn out to be irrelevant, science should be able to say so decisively.
If they turn out to be relevant—even partially—science should not arrive at that conclusion a decade late.
Either way, the status quo—rising young-onset colorectal cancer, paired with an underpowered research response to modern exposures—is no longer defensible.
Source notes for editors and researchers (supporting documentation)
-
Colorectal cancer became the most common cancer-related cause of death in people under 50 by 2023; overall under-50 cancer death rates fell substantially from 1990–2023, while colorectal cancer mortality increased annually since ~2005:
-
Pilot hypothesis on phones carried below the waist (50 cases / 50 controls), including the reported “four times” association and the ipsilateral-carrying pattern and timing debate:
-
NIEHS/NTP summary of animal evidence (tumor findings at high exposure levels; limits of applicability to humans; why it challenges “only heating matters” assumptions):
-
IARC classification of radiofrequency electromagnetic fields as “possibly carcinogenic to humans” (Group 2B):
-
NCI’s summary position on cell phones and cancer (evidence to date suggests cellphone use does not cause brain or other cancers in humans):
-
Reuters reporting on HHS launching a study and FDA removing older webpages described as containing “old conclusions”:
-
FDA’s current consumer-facing summary on cell phones and RF energy (including its statement about the weight of evidence and practical exposure-reduction language):
-
RF Safe’s description of the S4–MITO–spin framework (advocacy-driven mechanistic synthesis presented as testable):